by WV Caring | Feb 2, 2022 | Blog Articles, End of Life, Uncategorized
If seeing your family, ordering your affairs, and having end-of-life conversations concerning your last wishes is important to you––you’re not alone. Ninety percent of Americans desire some form of contact with their family before passing away, but only thirty percent...

by WV Caring | Sep 22, 2021 | About Us Articles, Blog Archive, Blog Articles, End of Life, Hospice Care
You’ve been working hard your whole life, and you deserve something that proves it. (Hospice) Since entering the workforce you’ve been paying into the Medicare Trust Fund, the national health insurance program for people 65 years and older. In fact, 1.45% of your...

by WV Caring | Apr 15, 2021 | Blog Articles, News, News Articles
END-OF-LIFE CARE CONVERSATIONS Ninety percent of Americans say that talking about their end-of-life care wishes is important, but only 30 percent are actually having these conversations. WV Caring has partnered with The Conversation Project, a national public...

by WV Caring | Apr 29, 2020 | Blog Articles
Everyone values a reliable support system. When life gets tough, you should be able to go to someone with confidence and trust that they will have your back. At WV Caring, we understand that having additional support for your loved one with an advanced illness can...
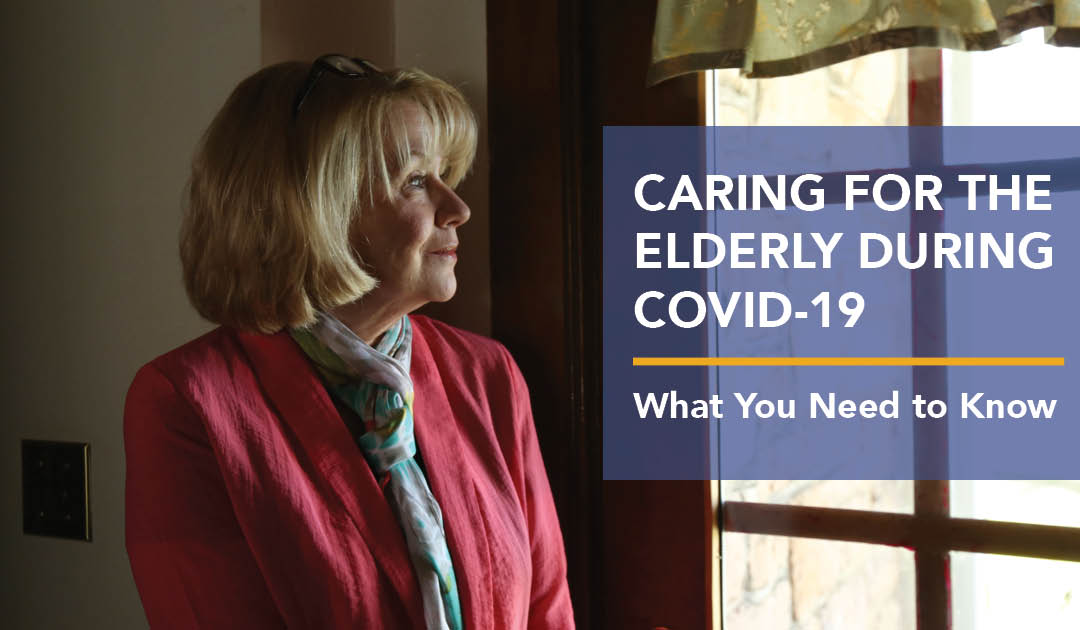
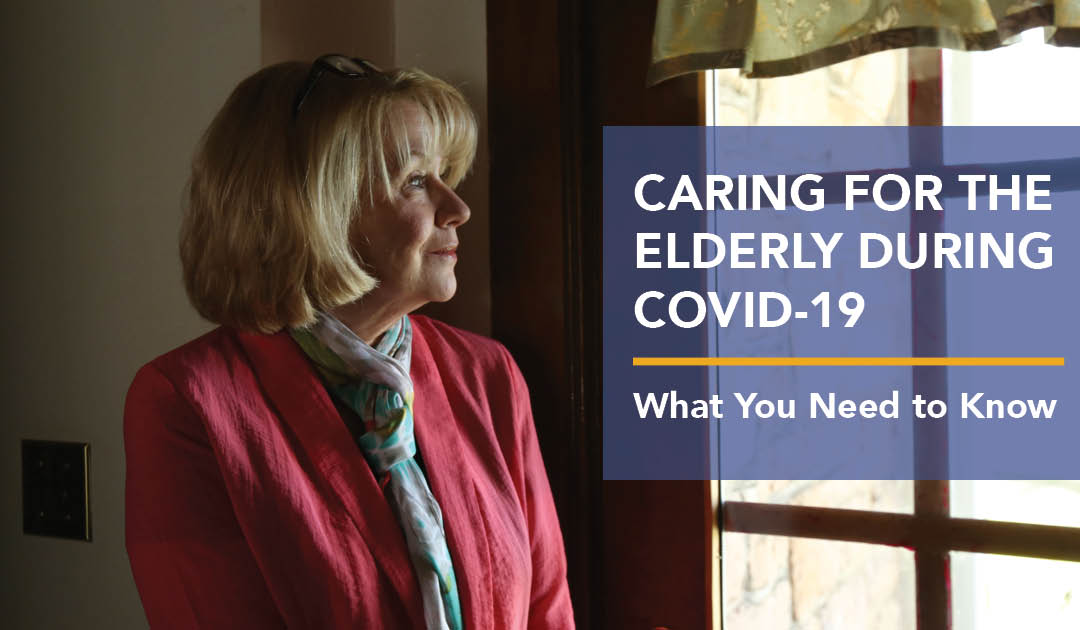
by WV Caring | Mar 26, 2020 | Blog Articles
During the coronavirus (COVID-19) pandemic, it is challenging to know what to do or how to take care of your loved one who may be at a higher risk of contracting this virus. This is especially true if they have an advanced illness. At WV Caring, our goal is to...
by WV Caring | Feb 21, 2020 | Blog Articles
Home, family, love, comfort, dignity, community and well-being are all signs of good, quality life. Excellent quality of life is what we would want for our loved ones with an advanced illness, right? WV Caring is committed to providing your loved one with the care...